Avian Bornavirus (ABV) is an enveloped single-strand RNA virus with worldwide distribution that is responsible for the condition we now know as Proventricular Dilatation Disease (PDD). This condition has been identified in psittacines since the 1970s, and it was originally described as Macaw wasting disease. The causative agent, ABV, was only recently identified in 2008, although many other questions regarding this condition still remain. While this disease has been identified in numerous types of birds, this article will be focusing on psittacines, or parrot species, as they are the most commonly seen birds in clinical practice.
The description given to the disease process that is caused by ABV is itself somewhat controversial and contested. The pathology of the disease involves nonpurulent inflammation of peripheral nerves. While the autonomic nerves of the gastrointestinal (GI) tract are commonly affected, this inflammatory process can also affect the central nervous system, as well as other organs entirely, leading to symptoms that may not be related to the GI tract at all. The classic presentation of PDD is a bird that is weak and lethargic, often with a normal appetite. If handled, the owner may notice a decrease in weight, but often this is not noted until there is a significant change. The plumage may appear dull or tattered, due to chronic malnutrition. Feces may contain undigested seeds or other food material, and vomiting or regurgitation is often noted. Most of these symptoms are identified in the more advanced stages of the disease. Symptoms not related to the GI tract may include ataxia, lameness, blindness, or even seizures. These may be seen concurrent with, or independent of GI changes. Sudden death has been reported, in the absence of clinical symptoms. This may be due to changes or irregularities in cardiac conductivity, although this has not been proven.
Signalment for PDD is quite varied and can include any psittacine, although African grey parrots, Amazons, cockatoos, macaws, and cockatiels appear overrepresented. No age predilection has been identified, although a study in the early 1990s found the average age of affected birds to be 3.8 years old. Latent periods are suspected to be possible, with lengths being quite variable. Single-housed birds have become symptomatic after years of no known contact with, or exposure to, infected individuals.
Differential diagnoses for confirmed proventricular dilatation are numerous and should be ruled out prior to making a diagnosis of PDD. A partial list should include bacterial or mycotic infections, particularly Macrorhabdus ornithogaster, neoplasia, parasitism, heavy metal toxicity, or a gastrointestinal outflow obstruction. While proventricular dilatation may be seen with these conditions, they do not typically cause thinning of the proventricular wall as PDD does. If changes to the wall are noted, they usually involve a thickening secondary to chronic inflammation.
Viral RNA has been identified in several bodily fluids and materials, including feces, urine, tears, and oral secretions. Due to these findings, transmission has been assumed to be fecal-oral route. Several studies have found varying degrees of success with this hypothesis. Infected birds introduced into clean flocks resulted in spread of the disease to some, but not all, birds. Other studies have shown that horizontal transmission through direct contact was not a sufficient route in immunocompetent birds. Often these patients will test positive for the virus on feathers, or skin biopsies, but will never seroconvert. Due to these findings, Piepenbring et al concluded that exposure most likely did not achieve persistent infection. This hypothesis has been strengthened by the fact that multiple reports have identified infected and non-infected birds living together for years, with no transmission.
At the time of this publication, transmission is not fully understood. Both horizontal and vertical transmission appear possible, but several variables are thought to affect each of these, including individual health of the patient, genotype of the virus, and any possible co-infections.
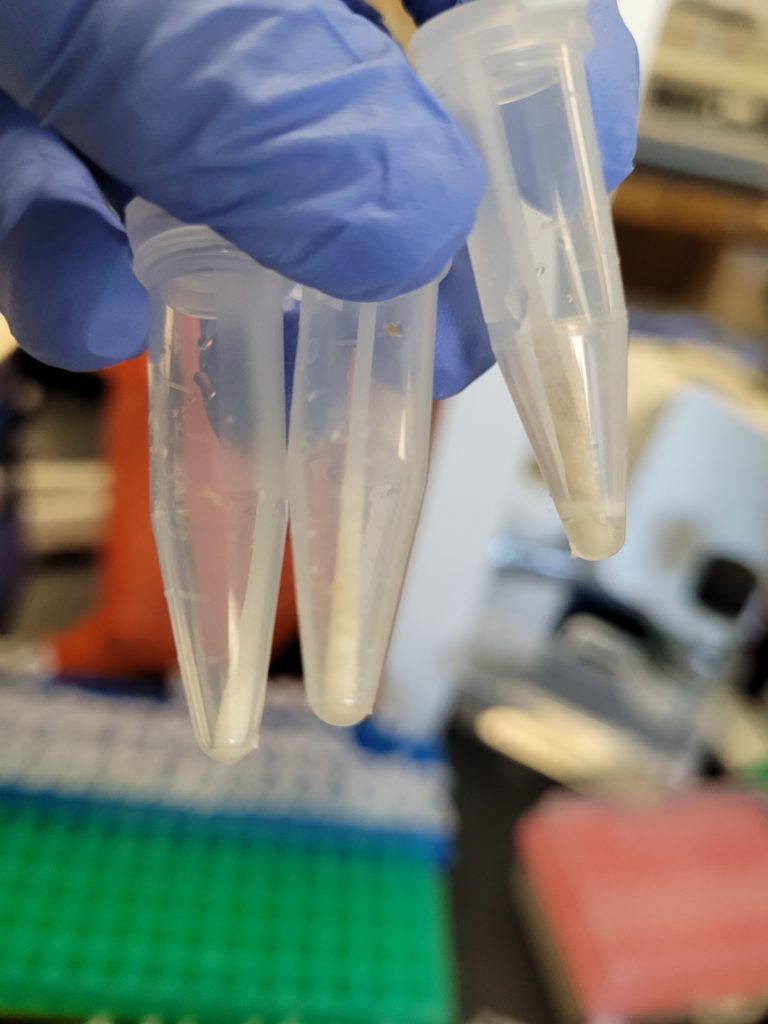
Diagnosis of a clinical ABV infection is, in a word, challenging. Initial detection of the virus in the living patient is typically done through reverse-transcription polymerase chain reaction (RT-PCR) testing. Samples submitted include cloacal/choanal swabs, tissue, and whole blood. Submitting a swab from only one site, or blood without accompanying swabs, dramatically reduced the likelihood of a positive sample. It is recommended to combine swabs and blood into one tube, although individual labs may have different submission requirements. Less commonly run tests to identify ABV include immunohistologic staining, and viral isolation. ABV-specific antibody detection (ELISA, Western blot) may provide valuable information for diagnosis, although at the present time it is unclear when antibodies are produced, or if they can potentially be correlated to clinical signs.
Another factor that adds even more confusion is the fact that some birds become infected with ABV, shed the virus, but never seroconvert. Several theories for why this may happen have been introduced, although none have been proven. Based on this information, the following protocols have been proposed to help identify positive and negative birds. A bird that is found to be positive for ABV using both PCR and serology should be considered a positive infection. A bird that is positive on PCR but negative on serology should be retested in 4-6 weeks to check for a false positive PCR and also to monitor for seroconversion. Repeated positive PCR tests and/or seroconversion should be considered a positive bird. Negative PCR paired with a positive serology are thought to be carriers, although this has not been proven. Persistent elevated titers are indicative of infection in mammals infected with bornavirus and should be considered the same for birds. Some birds appear to be able to clear the infection, which would explain the positive serology and negative PCR, although this, too, has yet to be proven.
Several therapies have been proposed for the treatment of both the symptoms of ABV, as well as for the virus itself. To date, there are no successful antiviral therapies reported. Previous reports of nonsteroidal anti-inflammatory drugs have failed to show significant, repeatable success. One study using meloxicam in infected cockatiels actually showed more severe lesions, and increased mortality, when compared to the control group. Immunosuppressive treatments, including the use of glucocorticosteroids, have been proposed at recent conferences. No published data has been made available as of yet, and clinicians should be cautious of these currently unproven methods. Symptomatic treatment, including diet modification, analgesia, and control of secondary infections, should be the basis of treatment for these cases.
Despite the recent advances in identifying and diagnosing this condition, there are still many questions left unanswered. While diagnostics have improved considerably, interpretation of these tests can still be challenging. A positive ABV diagnosis should not result in euthanasia, especially since many patients who test positive will never show symptoms. That being said, once patients become symptomatic, the chances of long-term survival are very low, and quality of life should be assessed. Along with the discovery of additional symptoms not related to the GI tract, some have proposed a name change from proventricular dilatation disease to avian or neuropathic ganglioneuritis. While this more accurately describes the condition, a name change has not been uniformly agreed upon at this time.
Which test is best, PCR or Serological Antibody?
A good method to determine whether your bird is actively producing the virus and thus capable of infecting other birds, including their progeny, is to run a PCR test on samples of droppings. Nonetheless, the antibody test might be helpful if you want to find out if a bird has ever been exposed to the virus before.
Gangliosides have been demonstrated as a potential marker for disease progression in birds with PDD/AG, even though testing for ABV is not specifically done with them. A potential technique for a more precise identification of clinically affected birds is serological testing for anti-ganglioside antibodies. To find out if your bird would benefit from this test, speak with your veterinarian.
How reliable are the tests for ABV and how do I interpret test results?
It is extremely unlikely for an ABV PCR test to yield a false-positive result. The bird most likely contains ABV if the PCR test comes back positive. But as previously stated, this DOES NOT imply that your bird will become ill.
Interpreting a negative PCR result from a fecal sample or cloacal swab can be more challenging. It indicates that on the day or days the samples were taken, your bird was not shedding the virus. This could be the result of either (A) the virus not infecting your bird or (B) the virus not actively being shed but still being present in the animal. Due to this sporadic shedding, it might be helpful to send several samples for PCR testing to ascertain whether a bird is infected.
You can probably assume your birds are not ABV-positive if they have a long history of good health, are rarely exposed to other birds, and you get negative PCR results. But if your bird exhibits symptoms and you think it might have ABV, speak with your veterinarian about doing further diagnostic testing.
PCR testing and serologic anti-ABV antibody testing yield quite different results. The bird has antibodies against ABV if the antibody test is positive. This implies that the bird developed an immune response after previously being exposed to ABV. It does not, however, indicate whether the birds are afflicted at this time.
A bird lacking antibodies against ABV is indicated by a negative antibody test. However, this could mean two very different things. It’s possible that the bird has never come into contact with or contracted ABV. As an alternative, it’s possible that the bird has contracted ABV but hasn’t yet developed an immunity to the virus. For these reasons, combining different testing techniques could yield a more definitive result regarding your bird’s ABV infection.


Generally speaking, sleepiness, fluffed or rumpled feathers when not cold, and decreased appetite are signs of illness in parrots (Left: Scarlet Macaw chick, Center: Blue-headed Pionus, and Left: Double Yellow-headed Amazon).
Is there a vaccine for ABV?
There is currently no vaccine against ABV. Research into developing a secure and reliable vaccine is presently being done by the Schubot Center and other research facilities.